At Canberra Surgicentre our surgeons undertake a variety of procedures under the specialty of Oral and Maxillofacial Surgery. You can find more information on each of these below.
Procedures
-
Oral
-
Cranio Maxillofacial
Removal of Wisdom Teeth
Wisdom teeth can become problematic when they are impacted, decayed or partially erupted, requiring surgical extraction.
What is an Impacted Wisdom Tooth?
A tooth becomes impacted due to lack of space in the dental arch and its eruption is therefore prevented by gum, bone, another tooth or all three. Lack of space occurs because our jaws have become smaller (through evolution), we do not loose teeth through decay as frequently as in the past, and our diet is such that our teeth do not wear down as much.
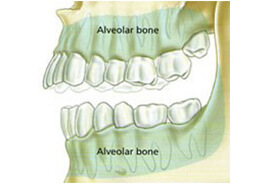
Diagram showing over-crowding of top jawline caused by erupting wisdom tooth. Note that the lower jawline has insufficient room for a wisdom tooth.
What are the indications for Removing Wisdom Teeth?
Wisdom teeth generally cause problems when they erupt partially through the gum. The most common reasons for removing them are:
- Decay– saliva, bacteria and food particles can collect around an impacted wisdom tooth causing it, or the tooth next to it, to decay. It is very difficult for the dentist to remove this decay and pain and infection will usually follow.
- Gum infection (pericoronitis) – when a wisdom tooth is partially erupted, food and bacteria collect under the gum causing a local infection. This may result in bad breath, pain, swelling and trismus (inability to open the mouth). The infection can spread to involve the cheek and neck. Once the initial episode occurs, each subsequent attack may become more frequent and severe.
- Pressure pain – pain may also come from the pressure of erupting wisdom teeth against other teeth. In some cases, this pressure may cause the erosion of the teeth immediately in front of the wisdom teeth.
- Orthodontic reasons– many younger patients have had prolonged orthodontic treatment to straighten teeth. Wisdom teeth may cause movement of teeth (particularly the front teeth) when they try to erupt and this will compromise the orthodontic result.
- Prosthetic reasons– patients who have had dentures constructed should have wisdom teeth removed. If a wisdom tooth erupts beneath a denture it may cause severe irritation, and if removed the patient may have to have another denture constructed to accommodate the changed shape of the gum.
- Cyst formation– a cyst (a fluid filled sack) can develop from the soft tissues which originally formed the wisdom tooth. Cysts cause bone destruction, jaw expansion and displacement and damage to the adjacent teeth. The removal of the cyst and tooth is necessary to prevent further bone loss. In rare circumstances, tumours may develop within these cysts or the jaw may even fracture if the cyst or tumour grows very large.
Travel to Inaccessible Place
If you are going to an area where specialist dental services are not available and your wisdom teeth are impacted, it may be advisable to have them removed beforehand.
Should an impacted wisdom tooth be removed if it hasn’t caused any trouble?
There is always a risk that impacted wisdom teeth may cause problems at any age. Such problems may occur suddenly and at inconvenient times. If the wisdom teeth appear to have a high probability of causing problems, your oral surgeon may advise you to have them removed.
When is the best time to have my wisdom teeth removed?
It is now recommended by specialists that if impacted wisdom teeth need to be removed, this is best done between the ages of 14 and 22 years. At this time surgery is technically easier, patients recover more quickly and the risk of complications is much lower. This is a relatively easy procedure in a patient at the age of 20, however it may become very difficult in a patient over 40 years of age.
Should a wisdom tooth be removed when an acute infection is present?
Generally, no. Surgery in the presence of infection can cause it to spread and become more serious. Firstly, the infection must be controlled with antibiotics, local oral hygiene and sometimes the extraction of the opposing wisdom tooth.
What type of anaesthetic should I have?
Wisdom teeth may be removed using local anaesthetic (LA) injections, LA injections and intravenous (IV) sedation or a general anaesthetic (GA). After discussing the advantages and disadvantages of each method with your oral surgeon, the choice depends on the number and difficulty of your wisdom teeth, any existing medical problems, and your own preference. Wisdom teeth can be removed with comfort by using either IV sedation and LA or GA and LA. Both procedures can be performed at Canberra Surgicentre.
How are impacted wisdom teeth removed?
Surgery is performed under sterile conditions, with all instruments sterilised using an autoclave. Both procedures IV and LA or GA and LA require the surgeon and assistant to wear a cap and mask together with a sterile gown and gloves. You will be required to wear a gown to ensure the protection of personal clothing.
Once satisfactory anaesthesia is achieved, surgery proceeds in the following sequence:
- the gum is incised (cut) and retracted to expose the tooth and adjacent bone.
- bone is removed with a drill to expose the tooth roots. In some cases it may be necessary to divide the tooth with a drill to allow its removal.
- following removal of the tooth, the wound is thoroughly cleaned.
- the wound is closed (stitched) with sutures which are usually dissolving.
What can I expect to happen after surgery?
Due to the local anaesthetic parts of your face will be numb for the first 2 to 3 hours after surgery. During this time you must be careful not to bite your lower lip and tongue.
It is normal to experience the following:
- Pain – bone is very sensitive to trauma and pain of moderate strength is a constant feature following removal of wisdom teeth. Strong analgesics will be prescribed and often need to be taken for at least three days after surgery.
- Swelling – this starts immediately after surgery and usually reaches its peak on the second day. It then reduces slowly over the following 3 to 4 days. Ice packs applied to the sides of the face for the first 8 hours (20 mins “on” and 20 mins “off”) help limit the swelling, reduce pain and decrease any residual bleeding.
- Bruising – this results from bleeding into the tissues. Some patients are more likely to bruise than others and it is not a serious problem.
- Jaw stiffness (trismus) – this occurs with swelling and will gradually diminish as the swelling resolves. This means that softer foods are more easily eaten during this period.
After surgery you will be given an INSTRUCTION SHEET to help you care for yourself at home. You will normally receive a prescription for an analgesic (to reduce discomfort) and an antibiotic (to help prevent infection).
What are the possible complications of having wisdom teeth removed?
Although not common, a number of potential complications are associated with the removal of wisdom teeth, and these include:
- Post operative infection– bacteria are a normal part of every mouth and they can cause an infection after wisdom tooth surgery. Antibiotics are always prescribed and good oral hygiene will help prevent this. Despite this, surgery sites can become infected in a small number of patients. Swelling, pain and limited jaw opening lasting more than 7 days may signal the presence of an infection.
- Dry socket formation– a dry socket is post extraction syndrome in which the blood clot in the tooth socket is lost. The symptoms include severe unrelenting pain usually commencing on the second or third day after a tooth is removed. It is NOT an infection, and is easily treated. Cigarette smoking is one suspected cause.
- Jaw joint dysfunction – occasionally the ligaments of the jaw joint become stretched as a result of having the mouth opened widely during surgery. A patient may experience some discomfort in and around the jaw joints and this may be relieved by applying heat (with a hot pack or water bottle) over the joint for 15 to 20 minutes twice daily. For more effective relief of discomfort, a non steroidal anti-inflammatory drug (soluble aspirin or Nurofen) may be used. Symptoms should resolve within 7 to 10 days.
- Nerve damage– an impacted wisdom tooth in the lower jaw is often very close to two nerves – the inferior alveolar and lingual nerves. The inferior alveolar nerve provides sensation to the lower lip and chin, and the lingual nerve provides sensation to the front part of the tongue on each side. Due to the close proximity of lower wisdom teeth to these nerves, they are occasionally injured during the removal of lower wisdom teeth – despite every precaution being taken to protect them during surgery. Bleeding in the area may also compress these nerves. Injury to these nerves may cause some numbness or tingling in the lip, chin or tongue after the local anaesthetic wears off. This numbness may take some weeks or months to resolve, and in a small number of cases it may be permanent. Your oral surgeon should be able, with the aid of your x-ray, to give you an indication if nerve damage is likely.
- Sinus opening – because the sinuses in the upper jaw are closely associated with the upper wisdom teeth, there is a small chance that when a wisdom tooth is removed, an opening into the sinus may be created. If this occurs and does not heal spontaneously, a second procedure may be necessary to close it.
- Bleeding – it is normal for there to be some residual oozing of blood from the surgery site for some hours after removal of wisdom teeth. If bleeding persists, pressure with gauze packs over the surgery site for about 1 hour may stop it. If it does not, you should contact your oral surgeon for advice.
The incidence of all complications after removal of wisdom teeth is in the order of 5% to 10%.
Any surgical or invasive procedure carries risks. Before proceeding, you should seek a second opinion from an appropriately qualified health practitioner.
Dental Implants
Dental implants can be placed as a permanent replacement for missing teeth providing a more permanent solution than dentures.
Who can benefit from Implantology?
Modern dentistry now offers hope for people who have missing or damaged teeth. If you are missing your natural teeth in one or both jaws and cannot wear dentures for physical or psychological reasons, we can offer you an innovative dental implant system that will provide most people with new teeth that look, feel and function like the real thing. People who are missing teeth may benefit from techniques that allow artificial teeth to be secured firmly in the mouth. These techniques range from replacing one missing tooth to replacing most teeth in the upper and lower jaws. People with loose teeth can also benefit from the insertion of implants as the tooth can be anchored into place. Implants can also be used to support removable dentures.
Dental Implants can offer a solution to people who have false teeth and want to avoid removable dentures. Many people have reported that dental implants have improved their appearance, have improved their chewing ability and are more comfortable.
Description
Dental implants are artificial substitutes for natural tooth roots as shown in the figures below:

The basic structure consists of the implant fixture and the prosthesis. The implant is a metal fixture that can be inserted into the jaw bone to provide a base for supporting and attaching the prosthesis. The prosthesis is an artificial tooth or row of teeth, which is attached to the implant/s. The prosthesis may be a “crown” to replace one missing tooth or a “bridge” to replace several missing teeth.
Compatibility
Implants are compatible with, and can bond strongly to bone tissue. Once teeth have already been removed, parts of the jaw bone that originally house the teeth have began to shrink. As the jawbone becomes smaller, there is less bone to comfortably anchor a denture. Once the implant is placed into the jawbone, shrinking stops and the bone stabilizes within the first year. The bone tissue grows onto the surface of the implant and when fixed firmly within the jaw bone, the implant will be strong enough to bear the daily forces of chewing and normal function. The implant procedure requires visits to our Consulting Rooms to plan healing and finally to attach the prosthetic tooth/teeth.
Options
 Implants are made of different materials such as metal titanium, and implanted in different ways. Each has its own advantages and disadvantages. You and your surgeon can discuss which implant system is likely to be best for you. Our surgeons use three brands of implants. These include Astra created by Astra Zeneca Group, the Branemark System created by Nobel Biocare and the Endopore Implant System created by Innova Technologies Corporation. We have chosen these specific brands of implants because of the many years of research behind the implants, the high quality and the success rate of patients who have received Branemark, Endopore and Astra implant systems.
Implants are made of different materials such as metal titanium, and implanted in different ways. Each has its own advantages and disadvantages. You and your surgeon can discuss which implant system is likely to be best for you. Our surgeons use three brands of implants. These include Astra created by Astra Zeneca Group, the Branemark System created by Nobel Biocare and the Endopore Implant System created by Innova Technologies Corporation. We have chosen these specific brands of implants because of the many years of research behind the implants, the high quality and the success rate of patients who have received Branemark, Endopore and Astra implant systems.
General Information
Patients need to be in good overall health, have healthy gums and sufficient bone to help support an implant. Regular dental visits and scrupulous oral hygiene are requisites for success. Dental Implants aren’t necessarily for everyone, your Surgeon will assess your suitability for this type of treatment.

Any surgical or invasive procedure carries risks. Before proceeding, you should seek a second opinion from an appropriately qualified health practitioner
TMJ Disorders
TMJ Disorders TMJ dysfunction is a common cause of orofacial pain. It can often be treated conservatively, but sometimes requires surgery.
What is the Temporomandibular Joint?
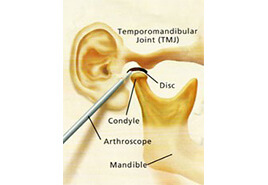
The temporomandibular joint (TMJ) connects the mandible (lower jaw) to the temporal bone (of the skull) at each side of the head just in front of the ear. Because these joints are flexible, the jaw can move smoothly up and down, side to side, forwards and backwards, thus enabling us to talk, chew and yawn. Muscles attached to and surrounding the TMJ control its position and movement. The hard and soft tissue components of the TMJ are somewhat unique in that when one moves then so does the other.
When the mouth is opened the rounded ends (condyles) of the lower jaw hinge and glide along the joint “sockets” of the temporal bone, returning to their original position when the mouth is closed. To keep this motion smooth, a soft “cartilage” disc lies in between the condyle and the temporal bone, and its main function is to absorb shocks to the TMJ from chewing, other movements and trauma.
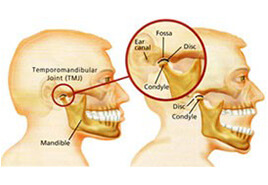
What is the Temporomandibular Joint?
The temporomandibular joint (TMJ) connects the mandible (lower jaw) to the temporal bone (of the skull) at each side of the head just in front of the ear. Because these joints are flexible, the jaw can move smoothly up and down, side to side, forwards and backwards, thus enabling us to talk, chew and yawn. Muscles attached to and surrounding the TMJ control its position and movement. The hard and soft tissue components of the TMJ are somewhat unique in that when one moves then so does the other.
When the mouth is opened the rounded ends (condyles) of the lower jaw hinge and glide along the joint “sockets” of the temporal bone, returning to their original position when the mouth is closed. To keep this motion smooth, a soft “cartilage” disc lies in between the condyle and the temporal bone, and its main function is to absorb shocks to the TMJ from chewing, other movements and trauma.
What are Temporomandibular Disorders?
It is generally agreed that TMJ disorders fall into three main categories:
- Internal derangement– any problem which does not allow the TMJ to function smoothly, but more specifically a problem with the position or structure of the disc.
- Myofascial pain – a common form of TMJ disorder that causes pain or discomfort in the muscles that control jaw function.
- Degenerative joint disease– conditions such as osteoarthritis or rheumatoid arthritis.
A person may have one or more of these conditions at the same time.
What Causes Temporomandibular Disorders?
The most common cause of temporomandibular joint disorders is trauma – either acute or chronic. It is well known that a severe acute injury to the jaw or TMJ may lead to a TMJ disorder – a heavy blow for example, may fracture bones within the joint or damage the disc thus disrupting the smooth motion of the jaw, causing pain and other symptoms. Symptoms may occur at the time of the injury and then resolve only to surface again at some time later. Degenerative joint disease may result from the injury.
The most common form of chronic trauma to the TMJ is believed to result from clenching the teeth. Stress, either physical or emotional, may cause a person to clench or grind their teeth at night during sleep – this habit may also occur during the day. The action of clenching tires the jaw muscles, puts undue load on the disc and ligament of the TMJ and may result in displacement of the disc and subsequent disabling symptoms.
Other causes of TMJ disorders are less clear. It has been suggested that a malocclusion (“bad bite”) may trigger the disorder, and orthodontic treatment which causes a movement of the teeth has also been blamed. Both these hypotheses are unlikely and have not been proven to be true.
What are the signs and symptoms?
The vast majority of patients who present for treatment of TMJ disorders are young females in the age range 15 to 35 years, but it is true to say that anyone may develop the disorder. A variety of symptoms develop and these may include:
- a clicking, popping or cracking sound in the joint.
- pain in and around the joint and associated jaw muscles.
- reduced mouth opening.
- headaches.
- dizziness.
- jaw locking – either open or closed.
- a disturbance in the “bite”.
- earaches and ringing or buzzing sounds.
Symptoms are often worsened when eating tough foods, yawning, in cold weather and in the morning on awakening. For most patients the condition will usually progress from a painless click in the joint, through joint pain to joint locking, although the time frame will vary enormously from patient to patient.
Diagnosis
Exact causes and symptoms of TMJ disorders may at times be unclear, diagnosis may be difficult and confusing. In the vast majority of cases, however, your description of symptoms, combined with a simple but comprehensive physical examination of the face, neck, jaws and mouth, will provide enough information to make a diagnosis.
The examination includes palpation of the TMJs and associated muscles in order to detect tenderness, listening for abnormal joint sounds, an analysis of jaw movement, and assessment of the teeth and bite. A careful check is also made of your medical and dental history.
An X-ray of the jaw, and particularly the TMJs, is usually requested to assess the status of the bony components of the joint. Other more complex X-ray techniques, such as arthrography (injection of a dye into the joint), computerised tomography (CT) or magnetic resonance imaging (MRI) may be requested if a more detailed examination of the joint is required, and particularly if the soft tissue components are to be visualised.
Treatment
It is most important to remember that most TMJ disorders will respond to simple conservative (non-invasive) treatment if a patient presents in the early phases of the condition. Conservative treatment is always used initially, and for a minimum of three months – after this period the majority of patients will respond fully or to a level where symptoms are manageable and tolerable.
Conservative treatments do not “invade” the tissues or alter the structure or position of the teeth. Simple treatments that your oral surgeon may advise are the basis of these conservative methods. Such treatments include:
- resting the jaw – avoiding tough foods and extreme jaw movements (such as yawning, loud singing and gum chewing).
- learning special techniques for relaxing, identifying and reducing stress.
- applying heat to the jaw joints (TMJ’s) by means of a hot water bottle or commercial heat packs twice daily for ten minutes each time, morning and night.
- physiotherapy in the form of ultrasound.
- pain relieving and anti-inflammatory drugs.
Perhaps the most important conservative measure is the construction of an occlusal (bite) splint. The splint is removable and is made of clear plastic and fits over the upper (usually) or lower teeth. The splint can help reduce the effects of clenching and grinding by keeping the teeth apart by a very small amount – the splint is about 2mm thick – and hence decreases the overload placed on the TMJ. Once the disc is “unloaded” it may regenerate to its normal position and function within the joint. The splint is usually worn only during sleep and does not cause permanent changes or damage to the bite or teeth.
Your progress is checked regularly during conservative treatment to assess responses and to enable a prognosis to be presented to you. It is important to remember that conservative treatment may not “cure” TMJ dysfunction permanently and symptoms may recur, particularly if clenching continues. If this occurs, further assessment is essential.
There are other forms of treatment for TMJ disorders that do not respond fully to conservative management. If symptoms persist at a level where a patient requests further treatment, your oral surgeon may recommend one or more of the following:
- an injection of a cortisone into the joint.
- an arthroscopic examination of the joint.
- an open surgical operation on the joint.
Surgical treatments may be irreversible and should be considered carefully by both patient and doctor. When such treatment is advised, your oral surgeon will carefully explain the possible alternatives, the side effects, possible complications and expected outcomes in words that you, the patient, can understand. Even when TMJ disorders have become chronic, most patients will not require or request more invasive methods of treatment and indeed the ultimate decision as to whether surgery is to be carried out rests with you, the patient, based on the advice given by your oral surgeon.
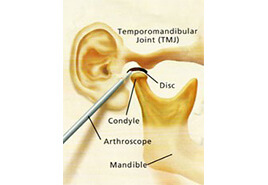
Arthrocentesis
Arthrocentesis may be utilised as a surgical intervention to treat TMJ dysfunction if conservative treatment is unsuitable.
Arthrocentesis is a relatively simple and minimally invasive procedure whereby a sterile needle and syringe are used to drain fluid from a joint.
Local anaesthetic is injected in the area of the joint. A needle with a syringe attached is inserted within the joint and fluid is sucked back (aspirated).
Joint fluid may be sent for examination to a pathologist to determine the cause of the joint swelling, such as infection, arthritis or gout.
The procedure is limited to restoring jaw function to a previously locked jaw. While admission to a Day Surgery facility is sometimes necessary, the procedure can be performed in our Consulting Rooms
Apicectomies
Apicectomies Apicectomy is a procedure in which a portion of the root of a tooth is removed either under sedation or local anaesthetic.
An apicectomy is a surgical procedure in which a portion of the root of a tooth is removed.
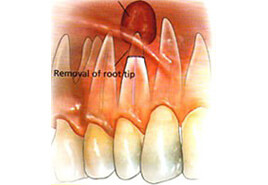 An apicectomy should not be considered an elective procedure, but should be undertaken only when conventional endodontic root filling techniques have failed. A conventional endodontic treatment (root canal therapy) is indicated if the dental pulp (nerve) of a tooth becomes non-vital (dies) or is likely to be put at risk due to the type or size of restoration needed to repair the tooth. During endodontic treatment the dental surgeon will remove the non-vital dental pulp from the tooth and replace it with an inert filling material which is visible on x-ray. Most teeth will respond satisfactorily to this type of treatment and be symptom free. Some however will require an apicectomy.
An apicectomy should not be considered an elective procedure, but should be undertaken only when conventional endodontic root filling techniques have failed. A conventional endodontic treatment (root canal therapy) is indicated if the dental pulp (nerve) of a tooth becomes non-vital (dies) or is likely to be put at risk due to the type or size of restoration needed to repair the tooth. During endodontic treatment the dental surgeon will remove the non-vital dental pulp from the tooth and replace it with an inert filling material which is visible on x-ray. Most teeth will respond satisfactorily to this type of treatment and be symptom free. Some however will require an apicectomy.
Why is an Apicectomy indicated?
There are quite a number of reasons why a conventional root canal treatment might fail and an apicectomy be recommended:
- overextended root fillings – occasionally the root filling material used in conventional endodontic treatment may extend through the end of the root of the tooth. This material will cause a reaction akin to an infection around the end of the root of the tooth.
- underfilling of the root canal – if this occurs, part of the non-vital dental pulp will remain and cause an infection around the end of the root of the tooth.
- fracture of an endodontic instrument – the instruments used during endodontic treatment are extremely fine and brittle, and occasionally they may fracture in the canal of the tooth. They should be retrieved during an apicectomy.
- where the end of the tooth curves sharply – in this situation the dental surgeon may not be able to get the instrument past this curvature and hence non-vital dental pulp will be left in the tooth and cause an infection. This part of the root will be removed in an apicectomy.
- repeated infection around the end of the root despite adequate endodontic treatment – when an infection has been long standing before conventional endodontic treatment is undertaken it may become self-perpetuating despite a root canal treatment. The area of infection is removed during an apicectomy.
- the root canal is obliterated – in older patients the root canals of teeth may become blocked by dentine and prevent the completion of conventional endodontic treatment.
- the presence of accessory root canals – some teeth have extremely small (usually not visible on x-ray) extra root canals towards the ends of their roots and this can not be instrumented in a conventional root canal treatment. An apicectomy will remove the part of the root in which these extra canals exist and hence remove the non-vital dental pulp contained therein.
- the repair of root perforations – perforations in the sides of the roots of teeth may arise from internal or external resorption or from instruments or metal posts placed in the canals of teeth. It is most difficult to repair these defects, even surgically, and a repair procedure may only be a temporary measure.
How is an Apicectomy carried out?
The procedure may be carried out using either a local anaesthetic, with or without intravenous sedation, or a general anaesthetic in a hospital operating theatre. The choice between the methods will depend upon the degree of difficulty of the procedure, your medical history, and your own personal choice. Most, however, are carried out using local anaesthetic with intravenous sedation.
During the procedure a small “window” is made (with a scalpel) in the gum over the root of the tooth. Using a dental drill, the area around the end of the root of the tooth is exposed to determine the amount of tooth root that should be removed. This portion of tooth root is then removed with the drill. Any infected tissue is removed from around the end of the root of the tooth. At this stage a decision is made to place a medicated filling material into the canal of the tooth – the decision to do so depends upon the seal of the root canal filling material. The gum is then placed into its original position and several stitches (usually dissolving) are placed to speed the healing process.
What happens after an Apicectomy?
It will generally take about five to seven days for you to recover fully from the procedure. During this time you will expect to experience the following side effects:
- pain – the discomfort requires the prescription of a moderate strength analgesic such as Panadeine Forte. You will probably need to use them for about 48 hours after the procedure.
- swelling – the gum around the surgical area and quite often the face will swell for the first few days and this is quite normal following such a surgical procedure.
- bruising – a small bruise may also occur on the skin of the face over the surgical area.
Healing within the bone and around the end of the root of the tooth should be expected to be complete within six months. This can easily be checked by your dental surgeon with an x-ray of the tooth.
Complications
An apicectomy is usually carried out due to the tooth being in a debilitated state and it is possible for the procedure not to be successful. If this is so, the tooth will again cause symptoms such as pain, swelling and gum boils. If this occurs, it is possible to re-apicoectomise the tooth in an attempt to save it. Should the procedure fail again it may be necessary to extract the tooth. Your oral surgeon will usually be able to give you a prognosis for the tooth at the first consultation and or when the apicectomy is carried out.
Things to keep in mind
It is now possible to perform root canal treatments on almost all teeth hence an apicectomy is also surgically possible. Although the procedure becomes technically more difficult on the posterior teeth – the failure rate of conventional endodontic treatment and apicectomy increases on the posterior teeth.
During conventional endodontic therapy the dental surgeon will take every care but occasionally the optimum results are not able to be achieved. If your dental surgeon recommends an apicectomy, it is because he feels that the tooth may be lost without it and that an apicectomy may be the only method of saving the tooth.
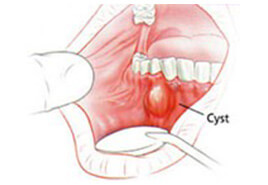
Minor Oral Procedures
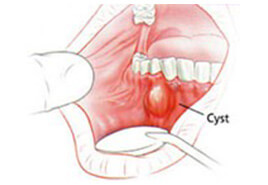
Removal of cysts of the jaw can be undertaken to avoid damage to teeth and often only require minor surgical intervention.
Cysts of the upper or lower jaw are fluid-filled sacs that can result in swelling, pain and infection.
The aim of treatment is to get rid of the cyst so that bone grows into the empty space. The most common surgical treatments are:
- enucleation – the cyst is opened and the lining of the cyst is removed.
- marsupialisation – the cyst is opened and only part of the lining is removed; a pouch is made so that the remainder of the lining becomes continuous with the tissue inside the mouth.
While the surgeon makes every attempt to save teeth involved with the cyst, one or more teeth may have to be removed, depending on the size and location of the cyst. Both procedures may be performed under Local, I.V. or General Anaesthetic
Oral Medicine and Pathology
A biopsy is a sample of the hard and soft tissues of the mouth, which your surgeon can send for histopathological diagnosis.
Oral and Maxillofacial Surgeons are able to accurately diagnose and treat medical conditions of the oral cavity and face.
Diseases of the oral cavity are sub-classified as to whether they are:
- congenital; or
- acquired.
Within disease categories it is not uncommon to diagnose inflammatory, immunological, infective, neoplastic (cancer), or drug related conditions of the mouth or face.
Forms of diagnosis may involve blood tests, biopsies, swabs, examination of salivary secretions and further tests as may be necessary.
The Oral and Maxillofacial Surgeon is both medically and dentally trained and is able to diagnose then treat the type of condition with the appropriate medication.
Oral Pathology
If abnormal tissue occurs in the mouth, a small piece may need to be removed by an oral maxillofacial surgeon for analysis.
This is called a biopsy. Tissue samples are taken by using a variety of cutting instruments.
The surgeon will send the tissue to a pathologist, a specialist in the diagnosis of abnormal tissue, who can also assess whether the tissue is non-cancerous (benign) or cancerous (malignant). The pathologist will then send a report to the surgeon, who will discuss the findings and options for further treatment with the patient. In some cases, a second biopsy may be needed to further refine diagnosis
Removal of Wisdom Teeth
Removal of Wisdom Teeth
Wisdom teeth can become problematic when they are impacted, decayed or partially erupted, requiring surgical extraction.
What is an Impacted Wisdom Tooth?
A tooth becomes impacted due to lack of space in the dental arch and its eruption is therefore prevented by gum, bone, another tooth or all three. Lack of space occurs because our jaws have become smaller (through evolution), we do not loose teeth through decay as frequently as in the past, and our diet is such that our teeth do not wear down as much.
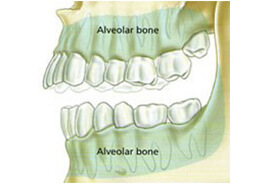
Diagram showing over-crowding of top jawline caused by erupting wisdom tooth. Note that the lower jawline has insufficient room for a wisdom tooth.
What are the indications for Removing Wisdom Teeth?
Wisdom teeth generally cause problems when they erupt partially through the gum. The most common reasons for removing them are:
- Decay– saliva, bacteria and food particles can collect around an impacted wisdom tooth causing it, or the tooth next to it, to decay. It is very difficult for the dentist to remove this decay and pain and infection will usually follow.
- Gum infection (pericoronitis) – when a wisdom tooth is partially erupted, food and bacteria collect under the gum causing a local infection. This may result in bad breath, pain, swelling and trismus (inability to open the mouth). The infection can spread to involve the cheek and neck. Once the initial episode occurs, each subsequent attack may become more frequent and severe.
- Pressure pain – pain may also come from the pressure of erupting wisdom teeth against other teeth. In some cases, this pressure may cause the erosion of the teeth immediately in front of the wisdom teeth.
- Orthodontic reasons– many younger patients have had prolonged orthodontic treatment to straighten teeth. Wisdom teeth may cause movement of teeth (particularly the front teeth) when they try to erupt and this will compromise the orthodontic result.
- Prosthetic reasons– patients who have had dentures constructed should have wisdom teeth removed. If a wisdom tooth erupts beneath a denture it may cause severe irritation, and if removed the patient may have to have another denture constructed to accommodate the changed shape of the gum.
- Cyst formation– a cyst (a fluid filled sack) can develop from the soft tissues which originally formed the wisdom tooth. Cysts cause bone destruction, jaw expansion and displacement and damage to the adjacent teeth. The removal of the cyst and tooth is necessary to prevent further bone loss. In rare circumstances, tumours may develop within these cysts or the jaw may even fracture if the cyst or tumour grows very large.
Travel to Inaccessible Place
If you are going to an area where specialist dental services are not available and your wisdom teeth are impacted, it may be advisable to have them removed beforehand.
Should an impacted wisdom tooth be removed if it hasn’t caused any trouble?
There is always a risk that impacted wisdom teeth may cause problems at any age. Such problems may occur suddenly and at inconvenient times. If the wisdom teeth appear to have a high probability of causing problems, your oral surgeon may advise you to have them removed.
When is the best time to have my wisdom teeth removed?
It is now recommended by specialists that if impacted wisdom teeth need to be removed, this is best done between the ages of 14 and 22 years. At this time surgery is technically easier, patients recover more quickly and the risk of complications is much lower. This is a relatively easy procedure in a patient at the age of 20, however it may become very difficult in a patient over 40 years of age.
Should a wisdom tooth be removed when an acute infection is present?
Generally, no. Surgery in the presence of infection can cause it to spread and become more serious. Firstly, the infection must be controlled with antibiotics, local oral hygiene and sometimes the extraction of the opposing wisdom tooth.
What type of anaesthetic should I have?
Wisdom teeth may be removed using local anaesthetic (LA) injections, LA injections and intravenous (IV) sedation or a general anaesthetic (GA). After discussing the advantages and disadvantages of each method with your oral surgeon, the choice depends on the number and difficulty of your wisdom teeth, any existing medical problems, and your own preference. Wisdom teeth can be removed with comfort by using either IV sedation and LA or GA and LA. Both procedures can be performed at Canberra Surgicentre.
How are impacted wisdom teeth removed?
Surgery is performed under sterile conditions, with all instruments sterilised using an autoclave. Both procedures IV and LA or GA and LA require the surgeon and assistant to wear a cap and mask together with a sterile gown and gloves. You will be required to wear a gown to ensure the protection of personal clothing.
Once satisfactory anaesthesia is achieved, surgery proceeds in the following sequence:
- the gum is incised (cut) and retracted to expose the tooth and adjacent bone.
- bone is removed with a drill to expose the tooth roots. In some cases it may be necessary to divide the tooth with a drill to allow its removal.
- following removal of the tooth, the wound is thoroughly cleaned.
- the wound is closed (stitched) with sutures which are usually dissolving.
What can I expect to happen after surgery?
Due to the local anaesthetic parts of your face will be numb for the first 2 to 3 hours after surgery. During this time you must be careful not to bite your lower lip and tongue.
It is normal to experience the following:
- Pain – bone is very sensitive to trauma and pain of moderate strength is a constant feature following removal of wisdom teeth. Strong analgesics will be prescribed and often need to be taken for at least three days after surgery.
- Swelling – this starts immediately after surgery and usually reaches its peak on the second day. It then reduces slowly over the following 3 to 4 days. Ice packs applied to the sides of the face for the first 8 hours (20 mins “on” and 20 mins “off”) help limit the swelling, reduce pain and decrease any residual bleeding.
- Bruising – this results from bleeding into the tissues. Some patients are more likely to bruise than others and it is not a serious problem.
- Jaw stiffness (trismus) – this occurs with swelling and will gradually diminish as the swelling resolves. This means that softer foods are more easily eaten during this period.
After surgery you will be given an INSTRUCTION SHEET to help you care for yourself at home. You will normally receive a prescription for an analgesic (to reduce discomfort) and an antibiotic (to help prevent infection).
What are the possible complications of having wisdom teeth removed?
Although not common, a number of potential complications are associated with the removal of wisdom teeth, and these include:
- Post operative infection– bacteria are a normal part of every mouth and they can cause an infection after wisdom tooth surgery. Antibiotics are always prescribed and good oral hygiene will help prevent this. Despite this, surgery sites can become infected in a small number of patients. Swelling, pain and limited jaw opening lasting more than 7 days may signal the presence of an infection.
- Dry socket formation– a dry socket is post extraction syndrome in which the blood clot in the tooth socket is lost. The symptoms include severe unrelenting pain usually commencing on the second or third day after a tooth is removed. It is NOT an infection, and is easily treated. Cigarette smoking is one suspected cause.
- Jaw joint dysfunction – occasionally the ligaments of the jaw joint become stretched as a result of having the mouth opened widely during surgery. A patient may experience some discomfort in and around the jaw joints and this may be relieved by applying heat (with a hot pack or water bottle) over the joint for 15 to 20 minutes twice daily. For more effective relief of discomfort, a non steroidal anti-inflammatory drug (soluble aspirin or Nurofen) may be used. Symptoms should resolve within 7 to 10 days.
- Nerve damage– an impacted wisdom tooth in the lower jaw is often very close to two nerves – the inferior alveolar and lingual nerves. The inferior alveolar nerve provides sensation to the lower lip and chin, and the lingual nerve provides sensation to the front part of the tongue on each side. Due to the close proximity of lower wisdom teeth to these nerves, they are occasionally injured during the removal of lower wisdom teeth – despite every precaution being taken to protect them during surgery. Bleeding in the area may also compress these nerves. Injury to these nerves may cause some numbness or tingling in the lip, chin or tongue after the local anaesthetic wears off. This numbness may take some weeks or months to resolve, and in a small number of cases it may be permanent. Your oral surgeon should be able, with the aid of your x-ray, to give you an indication if nerve damage is likely.
- Sinus opening – because the sinuses in the upper jaw are closely associated with the upper wisdom teeth, there is a small chance that when a wisdom tooth is removed, an opening into the sinus may be created. If this occurs and does not heal spontaneously, a second procedure may be necessary to close it.
- Bleeding – it is normal for there to be some residual oozing of blood from the surgery site for some hours after removal of wisdom teeth. If bleeding persists, pressure with gauze packs over the surgery site for about 1 hour may stop it. If it does not, you should contact your oral surgeon for advice.
The incidence of all complications after removal of wisdom teeth is in the order of 5% to 10%.
Any surgical or invasive procedure carries risks. Before proceeding, you should seek a second opinion from an appropriately qualified health practitioner.
Dental Implants
Dental Implants
Dental implants can be placed as a permanent replacement for missing teeth providing a more permanent solution than dentures.
Who can benefit from Implantology?
Modern dentistry now offers hope for people who have missing or damaged teeth. If you are missing your natural teeth in one or both jaws and cannot wear dentures for physical or psychological reasons, we can offer you an innovative dental implant system that will provide most people with new teeth that look, feel and function like the real thing. People who are missing teeth may benefit from techniques that allow artificial teeth to be secured firmly in the mouth. These techniques range from replacing one missing tooth to replacing most teeth in the upper and lower jaws. People with loose teeth can also benefit from the insertion of implants as the tooth can be anchored into place. Implants can also be used to support removable dentures.
Dental Implants can offer a solution to people who have false teeth and want to avoid removable dentures. Many people have reported that dental implants have improved their appearance, have improved their chewing ability and are more comfortable.
Description
Dental implants are artificial substitutes for natural tooth roots as shown in the figures below:

The basic structure consists of the implant fixture and the prosthesis. The implant is a metal fixture that can be inserted into the jaw bone to provide a base for supporting and attaching the prosthesis. The prosthesis is an artificial tooth or row of teeth, which is attached to the implant/s. The prosthesis may be a “crown” to replace one missing tooth or a “bridge” to replace several missing teeth.
Compatibility
Implants are compatible with, and can bond strongly to bone tissue. Once teeth have already been removed, parts of the jaw bone that originally house the teeth have began to shrink. As the jawbone becomes smaller, there is less bone to comfortably anchor a denture. Once the implant is placed into the jawbone, shrinking stops and the bone stabilizes within the first year. The bone tissue grows onto the surface of the implant and when fixed firmly within the jaw bone, the implant will be strong enough to bear the daily forces of chewing and normal function. The implant procedure requires visits to our Consulting Rooms to plan healing and finally to attach the prosthetic tooth/teeth.
Options
 Implants are made of different materials such as metal titanium, and implanted in different ways. Each has its own advantages and disadvantages. You and your surgeon can discuss which implant system is likely to be best for you. Our surgeons use three brands of implants. These include Astra created by Astra Zeneca Group, the Branemark System created by Nobel Biocare and the Endopore Implant System created by Innova Technologies Corporation. We have chosen these specific brands of implants because of the many years of research behind the implants, the high quality and the success rate of patients who have received Branemark, Endopore and Astra implant systems.
Implants are made of different materials such as metal titanium, and implanted in different ways. Each has its own advantages and disadvantages. You and your surgeon can discuss which implant system is likely to be best for you. Our surgeons use three brands of implants. These include Astra created by Astra Zeneca Group, the Branemark System created by Nobel Biocare and the Endopore Implant System created by Innova Technologies Corporation. We have chosen these specific brands of implants because of the many years of research behind the implants, the high quality and the success rate of patients who have received Branemark, Endopore and Astra implant systems.
General Information
Patients need to be in good overall health, have healthy gums and sufficient bone to help support an implant. Regular dental visits and scrupulous oral hygiene are requisites for success. Dental Implants aren’t necessarily for everyone, your Surgeon will assess your suitability for this type of treatment.

Any surgical or invasive procedure carries risks. Before proceeding, you should seek a second opinion from an appropriately qualified health practitioner
TMJ Disorders
TMJ Disorders
TMJ Disorders TMJ dysfunction is a common cause of orofacial pain. It can often be treated conservatively, but sometimes requires surgery.
What is the Temporomandibular Joint?
The temporomandibular joint (TMJ) connects the mandible (lower jaw) to the temporal bone (of the skull) at each side of the head just in front of the ear. Because these joints are flexible, the jaw can move smoothly up and down, side to side, forwards and backwards, thus enabling us to talk, chew and yawn. Muscles attached to and surrounding the TMJ control its position and movement. The hard and soft tissue components of the TMJ are somewhat unique in that when one moves then so does the other.
When the mouth is opened the rounded ends (condyles) of the lower jaw hinge and glide along the joint “sockets” of the temporal bone, returning to their original position when the mouth is closed. To keep this motion smooth, a soft “cartilage” disc lies in between the condyle and the temporal bone, and its main function is to absorb shocks to the TMJ from chewing, other movements and trauma.
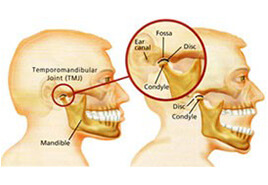
What is the Temporomandibular Joint?
The temporomandibular joint (TMJ) connects the mandible (lower jaw) to the temporal bone (of the skull) at each side of the head just in front of the ear. Because these joints are flexible, the jaw can move smoothly up and down, side to side, forwards and backwards, thus enabling us to talk, chew and yawn. Muscles attached to and surrounding the TMJ control its position and movement. The hard and soft tissue components of the TMJ are somewhat unique in that when one moves then so does the other.
When the mouth is opened the rounded ends (condyles) of the lower jaw hinge and glide along the joint “sockets” of the temporal bone, returning to their original position when the mouth is closed. To keep this motion smooth, a soft “cartilage” disc lies in between the condyle and the temporal bone, and its main function is to absorb shocks to the TMJ from chewing, other movements and trauma.
What are Temporomandibular Disorders?
It is generally agreed that TMJ disorders fall into three main categories:
- Internal derangement– any problem which does not allow the TMJ to function smoothly, but more specifically a problem with the position or structure of the disc.
- Myofascial pain – a common form of TMJ disorder that causes pain or discomfort in the muscles that control jaw function.
- Degenerative joint disease– conditions such as osteoarthritis or rheumatoid arthritis.
A person may have one or more of these conditions at the same time.
What Causes Temporomandibular Disorders?
The most common cause of temporomandibular joint disorders is trauma – either acute or chronic. It is well known that a severe acute injury to the jaw or TMJ may lead to a TMJ disorder – a heavy blow for example, may fracture bones within the joint or damage the disc thus disrupting the smooth motion of the jaw, causing pain and other symptoms. Symptoms may occur at the time of the injury and then resolve only to surface again at some time later. Degenerative joint disease may result from the injury.
The most common form of chronic trauma to the TMJ is believed to result from clenching the teeth. Stress, either physical or emotional, may cause a person to clench or grind their teeth at night during sleep – this habit may also occur during the day. The action of clenching tires the jaw muscles, puts undue load on the disc and ligament of the TMJ and may result in displacement of the disc and subsequent disabling symptoms.
Other causes of TMJ disorders are less clear. It has been suggested that a malocclusion (“bad bite”) may trigger the disorder, and orthodontic treatment which causes a movement of the teeth has also been blamed. Both these hypotheses are unlikely and have not been proven to be true.
What are the signs and symptoms?
The vast majority of patients who present for treatment of TMJ disorders are young females in the age range 15 to 35 years, but it is true to say that anyone may develop the disorder. A variety of symptoms develop and these may include:
- a clicking, popping or cracking sound in the joint.
- pain in and around the joint and associated jaw muscles.
- reduced mouth opening.
- headaches.
- dizziness.
- jaw locking – either open or closed.
- a disturbance in the “bite”.
- earaches and ringing or buzzing sounds.
Symptoms are often worsened when eating tough foods, yawning, in cold weather and in the morning on awakening. For most patients the condition will usually progress from a painless click in the joint, through joint pain to joint locking, although the time frame will vary enormously from patient to patient.
Diagnosis
Exact causes and symptoms of TMJ disorders may at times be unclear, diagnosis may be difficult and confusing. In the vast majority of cases, however, your description of symptoms, combined with a simple but comprehensive physical examination of the face, neck, jaws and mouth, will provide enough information to make a diagnosis.
The examination includes palpation of the TMJs and associated muscles in order to detect tenderness, listening for abnormal joint sounds, an analysis of jaw movement, and assessment of the teeth and bite. A careful check is also made of your medical and dental history.
An X-ray of the jaw, and particularly the TMJs, is usually requested to assess the status of the bony components of the joint. Other more complex X-ray techniques, such as arthrography (injection of a dye into the joint), computerised tomography (CT) or magnetic resonance imaging (MRI) may be requested if a more detailed examination of the joint is required, and particularly if the soft tissue components are to be visualised.
Treatment
It is most important to remember that most TMJ disorders will respond to simple conservative (non-invasive) treatment if a patient presents in the early phases of the condition. Conservative treatment is always used initially, and for a minimum of three months – after this period the majority of patients will respond fully or to a level where symptoms are manageable and tolerable.
Conservative treatments do not “invade” the tissues or alter the structure or position of the teeth. Simple treatments that your oral surgeon may advise are the basis of these conservative methods. Such treatments include:
- resting the jaw – avoiding tough foods and extreme jaw movements (such as yawning, loud singing and gum chewing).
- learning special techniques for relaxing, identifying and reducing stress.
- applying heat to the jaw joints (TMJ’s) by means of a hot water bottle or commercial heat packs twice daily for ten minutes each time, morning and night.
- physiotherapy in the form of ultrasound.
- pain relieving and anti-inflammatory drugs.
Perhaps the most important conservative measure is the construction of an occlusal (bite) splint. The splint is removable and is made of clear plastic and fits over the upper (usually) or lower teeth. The splint can help reduce the effects of clenching and grinding by keeping the teeth apart by a very small amount – the splint is about 2mm thick – and hence decreases the overload placed on the TMJ. Once the disc is “unloaded” it may regenerate to its normal position and function within the joint. The splint is usually worn only during sleep and does not cause permanent changes or damage to the bite or teeth.
Your progress is checked regularly during conservative treatment to assess responses and to enable a prognosis to be presented to you. It is important to remember that conservative treatment may not “cure” TMJ dysfunction permanently and symptoms may recur, particularly if clenching continues. If this occurs, further assessment is essential.
There are other forms of treatment for TMJ disorders that do not respond fully to conservative management. If symptoms persist at a level where a patient requests further treatment, your oral surgeon may recommend one or more of the following:
- an injection of a cortisone into the joint.
- an arthroscopic examination of the joint.
- an open surgical operation on the joint.
Surgical treatments may be irreversible and should be considered carefully by both patient and doctor. When such treatment is advised, your oral surgeon will carefully explain the possible alternatives, the side effects, possible complications and expected outcomes in words that you, the patient, can understand. Even when TMJ disorders have become chronic, most patients will not require or request more invasive methods of treatment and indeed the ultimate decision as to whether surgery is to be carried out rests with you, the patient, based on the advice given by your oral surgeon.
Arthrocentesis
Arthrocentesis
Arthrocentesis may be utilised as a surgical intervention to treat TMJ dysfunction if conservative treatment is unsuitable.
Arthrocentesis is a relatively simple and minimally invasive procedure whereby a sterile needle and syringe are used to drain fluid from a joint.
Local anaesthetic is injected in the area of the joint. A needle with a syringe attached is inserted within the joint and fluid is sucked back (aspirated).
Joint fluid may be sent for examination to a pathologist to determine the cause of the joint swelling, such as infection, arthritis or gout.
The procedure is limited to restoring jaw function to a previously locked jaw. While admission to a Day Surgery facility is sometimes necessary, the procedure can be performed in our Consulting Rooms
Apicectomies
Apicectomies
Apicectomies Apicectomy is a procedure in which a portion of the root of a tooth is removed either under sedation or local anaesthetic.
An apicectomy is a surgical procedure in which a portion of the root of a tooth is removed.
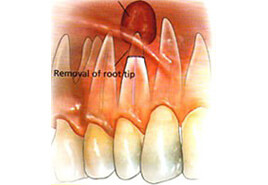 An apicectomy should not be considered an elective procedure, but should be undertaken only when conventional endodontic root filling techniques have failed. A conventional endodontic treatment (root canal therapy) is indicated if the dental pulp (nerve) of a tooth becomes non-vital (dies) or is likely to be put at risk due to the type or size of restoration needed to repair the tooth. During endodontic treatment the dental surgeon will remove the non-vital dental pulp from the tooth and replace it with an inert filling material which is visible on x-ray. Most teeth will respond satisfactorily to this type of treatment and be symptom free. Some however will require an apicectomy.
An apicectomy should not be considered an elective procedure, but should be undertaken only when conventional endodontic root filling techniques have failed. A conventional endodontic treatment (root canal therapy) is indicated if the dental pulp (nerve) of a tooth becomes non-vital (dies) or is likely to be put at risk due to the type or size of restoration needed to repair the tooth. During endodontic treatment the dental surgeon will remove the non-vital dental pulp from the tooth and replace it with an inert filling material which is visible on x-ray. Most teeth will respond satisfactorily to this type of treatment and be symptom free. Some however will require an apicectomy.
Why is an Apicectomy indicated?
There are quite a number of reasons why a conventional root canal treatment might fail and an apicectomy be recommended:
- overextended root fillings – occasionally the root filling material used in conventional endodontic treatment may extend through the end of the root of the tooth. This material will cause a reaction akin to an infection around the end of the root of the tooth.
- underfilling of the root canal – if this occurs, part of the non-vital dental pulp will remain and cause an infection around the end of the root of the tooth.
- fracture of an endodontic instrument – the instruments used during endodontic treatment are extremely fine and brittle, and occasionally they may fracture in the canal of the tooth. They should be retrieved during an apicectomy.
- where the end of the tooth curves sharply – in this situation the dental surgeon may not be able to get the instrument past this curvature and hence non-vital dental pulp will be left in the tooth and cause an infection. This part of the root will be removed in an apicectomy.
- repeated infection around the end of the root despite adequate endodontic treatment – when an infection has been long standing before conventional endodontic treatment is undertaken it may become self-perpetuating despite a root canal treatment. The area of infection is removed during an apicectomy.
- the root canal is obliterated – in older patients the root canals of teeth may become blocked by dentine and prevent the completion of conventional endodontic treatment.
- the presence of accessory root canals – some teeth have extremely small (usually not visible on x-ray) extra root canals towards the ends of their roots and this can not be instrumented in a conventional root canal treatment. An apicectomy will remove the part of the root in which these extra canals exist and hence remove the non-vital dental pulp contained therein.
- the repair of root perforations – perforations in the sides of the roots of teeth may arise from internal or external resorption or from instruments or metal posts placed in the canals of teeth. It is most difficult to repair these defects, even surgically, and a repair procedure may only be a temporary measure.
How is an Apicectomy carried out?
The procedure may be carried out using either a local anaesthetic, with or without intravenous sedation, or a general anaesthetic in a hospital operating theatre. The choice between the methods will depend upon the degree of difficulty of the procedure, your medical history, and your own personal choice. Most, however, are carried out using local anaesthetic with intravenous sedation.
During the procedure a small “window” is made (with a scalpel) in the gum over the root of the tooth. Using a dental drill, the area around the end of the root of the tooth is exposed to determine the amount of tooth root that should be removed. This portion of tooth root is then removed with the drill. Any infected tissue is removed from around the end of the root of the tooth. At this stage a decision is made to place a medicated filling material into the canal of the tooth – the decision to do so depends upon the seal of the root canal filling material. The gum is then placed into its original position and several stitches (usually dissolving) are placed to speed the healing process.
What happens after an Apicectomy?
It will generally take about five to seven days for you to recover fully from the procedure. During this time you will expect to experience the following side effects:
- pain – the discomfort requires the prescription of a moderate strength analgesic such as Panadeine Forte. You will probably need to use them for about 48 hours after the procedure.
- swelling – the gum around the surgical area and quite often the face will swell for the first few days and this is quite normal following such a surgical procedure.
- bruising – a small bruise may also occur on the skin of the face over the surgical area.
Healing within the bone and around the end of the root of the tooth should be expected to be complete within six months. This can easily be checked by your dental surgeon with an x-ray of the tooth.
Complications
An apicectomy is usually carried out due to the tooth being in a debilitated state and it is possible for the procedure not to be successful. If this is so, the tooth will again cause symptoms such as pain, swelling and gum boils. If this occurs, it is possible to re-apicoectomise the tooth in an attempt to save it. Should the procedure fail again it may be necessary to extract the tooth. Your oral surgeon will usually be able to give you a prognosis for the tooth at the first consultation and or when the apicectomy is carried out.
Things to keep in mind
It is now possible to perform root canal treatments on almost all teeth hence an apicectomy is also surgically possible. Although the procedure becomes technically more difficult on the posterior teeth – the failure rate of conventional endodontic treatment and apicectomy increases on the posterior teeth.
During conventional endodontic therapy the dental surgeon will take every care but occasionally the optimum results are not able to be achieved. If your dental surgeon recommends an apicectomy, it is because he feels that the tooth may be lost without it and that an apicectomy may be the only method of saving the tooth.
Minor Oral Procedures
Minor Oral Procedures
Removal of cysts of the jaw can be undertaken to avoid damage to teeth and often only require minor surgical intervention.
Cysts of the upper or lower jaw are fluid-filled sacs that can result in swelling, pain and infection.
The aim of treatment is to get rid of the cyst so that bone grows into the empty space. The most common surgical treatments are:
- enucleation – the cyst is opened and the lining of the cyst is removed.
- marsupialisation – the cyst is opened and only part of the lining is removed; a pouch is made so that the remainder of the lining becomes continuous with the tissue inside the mouth.
While the surgeon makes every attempt to save teeth involved with the cyst, one or more teeth may have to be removed, depending on the size and location of the cyst. Both procedures may be performed under Local, I.V. or General Anaesthetic
Oral Medicine and Pathology
Oral Medicine and Pathology
A biopsy is a sample of the hard and soft tissues of the mouth, which your surgeon can send for histopathological diagnosis.
Oral and Maxillofacial Surgeons are able to accurately diagnose and treat medical conditions of the oral cavity and face.
Diseases of the oral cavity are sub-classified as to whether they are:
- congenital; or
- acquired.
Within disease categories it is not uncommon to diagnose inflammatory, immunological, infective, neoplastic (cancer), or drug related conditions of the mouth or face.
Forms of diagnosis may involve blood tests, biopsies, swabs, examination of salivary secretions and further tests as may be necessary.
The Oral and Maxillofacial Surgeon is both medically and dentally trained and is able to diagnose then treat the type of condition with the appropriate medication.
Oral Pathology
If abnormal tissue occurs in the mouth, a small piece may need to be removed by an oral maxillofacial surgeon for analysis.
This is called a biopsy. Tissue samples are taken by using a variety of cutting instruments.
The surgeon will send the tissue to a pathologist, a specialist in the diagnosis of abnormal tissue, who can also assess whether the tissue is non-cancerous (benign) or cancerous (malignant). The pathologist will then send a report to the surgeon, who will discuss the findings and options for further treatment with the patient. In some cases, a second biopsy may be needed to further refine diagnosis
Corrective Jaw Surgery
What is Orthognathic Surgery?
As orthodontics is concerned with the correct alignment of the teeth, so orthognathic surgery encompasses those procedures that are used to place the jaws in their correct position. Usually the two specialities are carried out in close co-operation and often simultaneously. Close cooperation will therefore take place between your orthodontist, dental surgeon and oral maxillofacial surgeon.
Orthognathic surgery is a well established and recognised field of oral and maxillofacial surgery with many of the procedures being developed as early as the 1920’s. Great advances have taken place since the 1960’s with perhaps the most important being the introduction of rigid internal fixation methods (small metal bone plates) which have made the practice of wiring the jaws together in the immediate post-surgical recovery period less common.
During your consultations with your surgeon it is important that you ask as many questions as you feel are necessary to increase your understanding of this procedure. Parents and spouse are also encouraged to attend consultations. During the consultations, your surgeon will discuss the diagnosis of your particular case, using your dental records, x-rays and other visual aids as are necessary. The purpose of the pre-operative consultations is to provide you with as much specific information as possible to enable you to understand the procedures and to allow you to make an informed decision about your treatment.
Corrective Jaw Surgery – before and after examples

Orthognathic Surgery and Orthodontics
Many malocclusions (the improper alignment of upper and lower teeth) are corrected by wearing braces alone. In some situations, however, the upper and lower jaws are of a different size or shape, or are in an incorrect relationship to one another, and in this circumstance orthodontic treatment alone may not be able to align the upper and lower teeth. In this situation your orthodontist may suggest that orthognathic surgery will be necessary to align the jaws and hence the teeth so that the orthodontic result is not compromised and so that the optimum result is achieved as far as long-term stability, appearance and function are concerned. Following a detailed study of your particular case using dental models, x-rays, computer tracings and predictions, your orthodontist and oral maxillofacial surgeon will be able to recommend the best programme of combined treatment.
The Sequence of Treatment
Combined orthodontic and surgical treatment often takes considerable time to complete and therefore requires great motivation and cooperation from the patient, as well as a close liaison between you, your orthodontist and oral maxillofacial surgeon. Several stages are involved in treatment:
The timing of the various stages is usually controlled by your orthodontist but it may be quite possible to organise the surgical treatment around school, work, family and social life.
- Treatment Planning– begins with an initial consultation with your orthodontist. If surgery is recommended your oral maxillofacial surgeon and orthodontist will work closely together to plan the program of treatment, using dental plaster models, x-rays, photographs, computer tracings and predictions. No treatment will be instituted until you are fully informed and have consented to the proposed program.
- Pre-Surgical Orthodontic Treatment – before surgery can be undertaken it will be necessary to align the teeth in each jaw. Due to the malalignment of the jaws, the occlusion (the way in which the teeth meet) at this stage will not be correct. The purpose of pre-surgical orthodontics is to allow the plaster dental models to be examined so that correct alignment of the teeth is assured at the time of surgery.
- Surgical Treatment – prior to having your braces placed, or even during the pre-surgical phase of orthodontic treatment, it may be necessary to have several teeth extracted as they would interfere with the main orthognathic procedure. The most important teeth to be removed are the wisdom teeth, and your oral maxillofacial surgeon will usually carry out this operation. It is advisable to have them removed at least three months prior to the orthognathic surgery to allow adequate bone healing to take place.Once your teeth have been sufficiently straightened, you will have another consultation with your oral maxillofacial surgeon so that details of the operation, your stay in hospital and the recovery period are fully understood.Orthognathic surgery is performed in a hospital operating theatre under a general anaesthetic. Usually, you will be admitted to the hospital on the day before surgery and be discharged home on the morning of the third or fourth post-operative day. The anaesthetist will examine you in hospital and explain what is involved in a general anaesthetic. All modern orthognathic procedures are carried out through the mouth using high speed air-driven bone cutting saws and titanium mini bone plates and screws. Upper jaw surgery is completed entirely within the mouth as is lower jaw surgery but with a small (3mm) incision made on the side of the cheek. These “stab” incisions are used to insert the bone screws and will heal to an “invisible” scar within a few weeks. When lower jaw surgery is carried out, a thin plastic drain tube may be led out through the cheek on each side to reduce the amount of facial swelling – the drain tubes are usually removed on the second day after surgery. Immediately at the completion of the operation and before you leave the operating theatre, elastic bands or wires will be placed between the upper and lower teeth to support the jaws in their new position. Generally these elastic bands or wires remain in place for several weeks after the operation.Your oral maxillofacial surgeon will see you every week for several weeks after surgery to assess your post-operative progress and you will see the orthodontist about one month after surgery to begin the post-surgical phase of orthodontic treatment.
- Post-Surgical Orthodontic Treatment – after healing has taken place and the new position of your jaw is stable, further orthodontic treatment will be carried out to enable the final position of the teeth to be obtained. Your orthodontist will tell you how long this stage will take.
Side Effects of Orthognathic Surgery
As this type of surgery is considered quite major it is not without a number of known and predictable temporary side effects.
- Pain – it is not uncommon for patients to experience more pain after the removal of wisdom teeth than after orthognathic surgery. Appropriate analgesics are given to you in hospital and to take home.
- Facial swelling– swelling on the face commences immediately after surgery and reaches a peak at about 48 hours. It does not begin to decrease significantly for about one week after the operation.
- Bruising – it is quite normal for some patients to have some bruising on the sides of the face, under the eyes and in the upper neck, and usually this occurs about one week after the operation. It may take another week to disappear.
- Jaw stiffness – because of the amount of swelling that occurs it is normal for the jaws to be somewhat stiff for about ten days after the operation.
- Dietary modification – it takes bone some time to regain enough strength after orthognathic surgery to allow a return to normal diet. During the first two weeks after the operation it is essential that all food is pureed. During the following two weeks only soft foods may be eaten. From the fourth week a gradual return to a normal diet may take place over the next two weeks. This is perhaps the most important aspect of post-operative recovery, advice will be given to you by a dietician prior to your discharge from hospital.
Complications of Orthognathic Surgery
Following the consultation with your surgeon, you will be given a summary of the procedure. The information provided is intended more to inform you, rather than to alarm you. The complications associated with the various drugs and medicines are too numerous to discuss in this page and perhaps you might discuss this with your anaesthetist who will meet with you, in hospital, before your operation.
- Haemorrhage (bleeding)– this may occur during or after the operation. Reactionary haemorrhage occurs in the first 24 hours after surgery, and secondary haemorrhage occurs 5 to 7 days after the operation and is usually the result of infection. If bleeding is excessive during an operation a transfusion may be required. If you or your family (i.e. immediate blood relatives) have any concern that there may be a bleeding disorder in the family, advise your oral maxillofacial surgeon of this concern in order that appropriate blood tests can be arranged promptly with a large and experienced pathology laboratory. If there is an abnormality, you will be referred to a haematologist for further assessment. If you have had unexplained bleeding associated with any operation, please share the details with your oral maxillofacial surgeon. Haematoma (a blood collection in the tissues) formation occurs in approximately 1-2% of operations on the jaw, and it is for this reason that surgical drains may be used.
- Wound infection – whilst this is quite uncommon in upper or lower jaw osteotomies, it is recognised. It is essential that you maintain scrupulous oral hygiene both before and after the operation. A prophylactic (scale and clean) is recommended by your dentist before your operation. Wound infection may be minor, small abscess or redness of the skin, or it may be serious or life-threatening. Your consultant anaesthetist will commence intravenous antibiotic therapy after the induction of the general anaesthetic and will be continued during your stay in hospital. After discharge you will also take oral antibiotics.
- Lung complications – if you are an asthmatic or smoker there is increased risk of lung complications, your oral maxillofacial surgeon will encourage you to stop smoking. This may be difficult and require you to discuss with your family doctor the use of a nicotine patch and/or Nicorette chewing gum. Physiotherapy may be required to encourage lung function in the immediate postoperative period.
- Thromboembolic phenomena – deep venous thrombosis (DVT) may occur in the veins of the legs and pelvis during surgery. Venous return of the blood from the legs to the heart is encouraged by electrical calf stimulation during the operation. Please be reassured the hospital has the necessary apparatus to deal with this. You may also wear TED (thromboembolic deterrent) stockings for approximately 5 days, and the nursing staff will encourage your early ambulation. Women taking the contraceptive pill should understand that there is an increased risk of venous thrombosis. In head and neck surgery pulmonary embolus (clot in the lungs) is relatively uncommon. Patients with previous history of venous thrombosis must inform your surgeon and your anaesthetist prior to surgery to ensure an appropriate drug is given to thin the blood. There are a number of drugs available, and your surgeon/anaesthetist will make this decision on your behalf. Please do not start taking one of these agents without advising your surgeon or anaesthetist. Failure to do so may result in your operation having to be rescheduled.
- Urinary tract – whereas post operative retention of urine tends to be more common in the older male patient, it does occur in young men and women, and if necessary a urinary catheter will be placed using a suitable anaesthetic jelly which permits the procedure without undue discomfort. Urinary tract infections may occur, and if you have a history of these infections, please tell your doctor. If the operation planned becomes prolonged (4-5 hours), you may be catheterised while you are under anaesthetic.
- Anaesthetic complications– these should be discussed with the anaesthetist, who will be pleased to discuss what is involved. You must be absolutely frank with your doctor about all and any problems relating to your health.
- Blood products – our surgical practice may arrange for autologous (i.e. your own) blood to be available for elective operations, and the details will be discussed if necessary. If you have any reason to believe that you might be in a high risk group for hepatitis B or C, or the human immunodeficiency virus, HIV-AIDS, please discuss it in confidence with the surgeon. You will not be discriminated against, but we do need to know in order that additional safeguards may be set in place for your safety and wellbeing and that of your health care workers.
- Bedsores– pressure sores result from compression of the skin covering over a prominent bony part of the body. Whilst such pressure sores are uncommon in younger patients, there is higher incidence amongst the elderly, who are particularly susceptible. Pressure sores generally occur more commonly on the lower half of the body, over the tail bone, hip and heel. Please be reassured the nursing staff at the hospital have great experience in pressure sore prevention.
- Local complications:
- the incisions and result scars – jaw osteotomies are carried out through incisions in the mouth. The incisions are made in the mucosal lining usually at the junction of cheek and lip with the upper or lower jaw. Dissolving stitches are used. If any scarring occurs it is not visible from the outside. For lower jaw surgery there will be a tiny (3mm) “stab” incision in each cheek (at the angle of the jaw). These incisions generally heal to virtually invisible scars within a month or two after the operation, although rarely there may be a small depression or tiny scar remaining. However, if you are a person who has in the past, formed poor, hypertrophic or keloidal scars, it does not necessarily mean that you will form a prominent scar in association with this operation. Great care is taken during the operation with gentle tissue handling. If a bone graft has been used from the hip, the scar will remain a little conspicuous for 6 to 8 months and it will never disappear entirely.
- nerve injuries– there are many nerves crisscrossing the face and neck, and two of these are of particular importance in jaw osteotomies.
- trigeminal nerve – this nerve is divided into three parts, and the lower two parts are at risk during the operations of upper and lower jaw. The nerve is dissected out over a distance of approximately 4cm. As a consequence, both these nerves on the right and left sides of the lower jaw are equally at risk. Even handling the nerve gently is sufficient to give rise to anaesthesia or numbness of the right and/or the left sides of the lower lip and chin. This condition is called a sensory neuropathy, and may take the form of numbness, pins and needles, burning, or even itching or the sensation of ants crawling across the skin. It is expected that all patients who have lower jaw osteotomies will have numbness in the lower lip and chin in the immediate post operative period. In most cases this numbness is temporary and usually wears off over a period of time several weeks to several months-sometimes up to 12 months. Very occasionally, however, the sensory neuropathy is permanent. The infra orbital nerves exit the upper jaw just below the lower rim of the eye socket and are also dissected out during operations on the upper jaw. Numbness is usual after an operation on the upper jaw in an area beneath the eye and extending down onto the upper lip and gums above the upper anterior teeth. This numbness is virtually always temporary (as above) and has a very low risk of being permanent. It is not uncommon for a patient who has undergone a maxillary osteotomy to complain that the gum immediately above the teeth between the gum line and the scar feels a little numb for months following the operation, and occasionally this is permanent. The patient may also complain that the teeth in the upper jaw “feel different” following the surgery.
- the lingual nerve –is responsible for sensation to the front two-thirds of the tongue, and the special sense of taste. Again, both the right and the left sides are at small risk during the operation of lower jaw osteotomy. The lingual sensory neuropathy is not common in mandibular osteotomy but it is a recognised complication and particularly as a result of nerve stretching or bruising of the nerve by retraction or screw positioning.
Bone grafts
Occasionally a bone graft is required and this will always be discussed in the preoperative consultation with your surgeon. The common sites used as the donor area are the hip and rib. If the hip graft is to be used, a separate explanation will be provided, depending on whether it is a vascularised or free graft. It if is a rib graft that is to be used, it will be harvested in the region of the 5th, 6th or 7th rib, and via a submammary incision. In a woman the incision will be carefully placed at the lower pole of the breast disc in the inframammary fold. A firm brassiere should be used in the month following surgery to provide pressure on the scar. Whilst perforation of the pleura (i.e. the lining membrane of the lung) is not common, it may occur, and require a chest drain in the post operative period. The use of a small catheter placed at the time of surgery allows the wound to be irrigated with a tiny dose of a long-acting local anaesthetic solution (Marcain), and this permits the patient to cough and move about the bed without undue discomfort or pain.
Other Complications
- Relapse – with the advent of rigid fixation using bone plates and screws this is not the problem that it was 15-20 years ago. Relapse may be due to a number of factors, and this will be discussed at the clinic. Generally speaking, the larger the jaw movements, the greater is the chance and degree of relapse. It is expected that there may be up to a 10% relapse after jaw osteotomies but this is usually accommodated for in the planning of the operation. Relapse may also occur after removal of the orthodontic bands and braces, and this is a matter that should be discussed with your consultant orthodontist.
- Temporomandibular joint – the patient with an established internal derangement with jaw joint pain, clicking, earache, locking and unlocking may require treatment prior to and after jaw osteotomy. The osteotomy may improve the function of the joint. It may have no effect on the function, or it may make it worse, necessitating further treatment, nonoperative or operative, on the jaw joint. This will be discussed at the consultation rooms. The patient with the asymptomatic jaw joint is in the majority, but occasionally an asymptomatic or silent jaw joint dysfunction may be unmasked as a consequence of the surgery. Rarely, jaw joint dysfunction may be unmasked by other surgery requiring endotracheal intubation. It should be most strongly emphasised that the anaesthetic has not caused the problem, but has unmasked the pre-existing but asymptomatic jaw joint problem. Almost invariably simple conservative measures of treatment involving splint therapy are all that is required.
Clearly it is not possible to provide patients with each and every complication associated with the operation, and some are extremely rare. The object of this page is to inform you of the important and material complications about which you or your family may wish to ask further questions, or which may decide you to postpone the operation to permit further discussion, or even to seek a second opinion. Please do not leave your questions until the night before the operation, as this may necessitate rescheduling of the operation. If you have a concern, contact our consulting rooms and advise our staff that you wish to discuss it once again with your oral maxillofacial surgeon. Finally, please remember to bring all the x-ray films, CAT, MRI or nuclear scans, to the hospital when you are admitted.
Consent Form
If you do not understand any aspect of this form, please feel free to discuss it well prior to the operation.
Some Important Facts to Remember
- Oral hygiene– it is absolutely essential that the mouth is kept scrupulously clean after orthognathic surgery. The use of mouthwashes after every meal is strongly recommended.
- Psychological considerations– It is not unusual for patients to become a little depressed after orthognathic surgery because of the early slow progress and the fact that it is difficult to see any results in the early stages due to facial swelling. This feeling will pass as you recover from surgery and the improvements in appearance and function become more apparent.
- Cost – it is important to discuss the expenses that will be incurred during treatment. Many of the costs will be partly covered by Medicare and your private medical fund but there will still be a gap.
